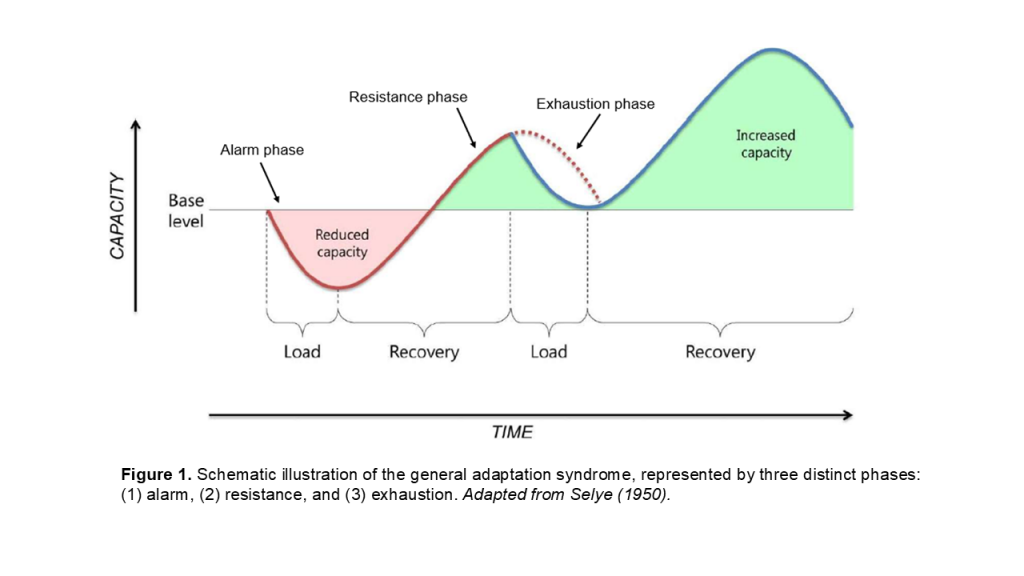
In the 1930’s, Hungarian scientist Hans Selye proposed the general adaptation syndrome – three distinct phases of how a range of body systems respond to stress. These distinct phases which were later expanded upon [4], include (1) an initial alarm phase, (2) a subsequent stage of resistance, where adaptation to the stressor occurs, and finally (3) exhaustion (or death), where tolerance to the stressor is lost. The general adaptation syndrome is commonly used to describe how humans respond and adapt to training stress (Figure 1).
Not All Load is Created Equally – and Not All Responses Follow the Same Timeline of Recovery!
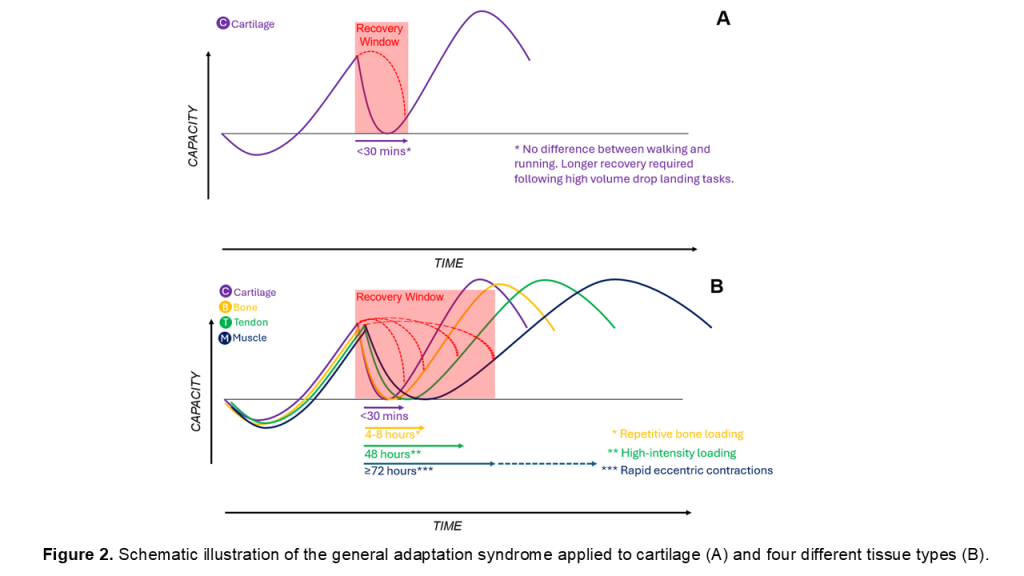
It is well-established that after an initial training dose, performance is reduced, followed by a return to performance at, or above (i.e. supercompensation) the initial levels. Although Selye [4] suggested that adaptation to stress is highly predictable, researchers have demonstrated that the biochemical response of a tissue depend on the type of training that is performed [5]. Importantly, these recovery timelines differ among cartilage, tendon, muscle and bone [3].
In our recent Sports Medicine paper, we detailed the different recovery durations of specific tissues and systems and highlighted the important role of volume and intensity upon these responses [3]. Although cartilage (<30 mins) and bone (~4-8 hours) can recover quickly following walking and running activities, extended periods of recovery are required following high-intensity tendon loading involving stretch-shortening activity (~48 hours) and muscle contractions involving eccentric activity (≥72 hours).
Could We Frame the Tissue Response to Load Within Selye’s General Adaptation Syndrome Framework?
An understanding of the general adaptation syndrome and tissue-specific load-responses can help practitioners design more effective rehab and peak performance programs. But how would specific tissues fit within the general adaptation syndrome framework? Figure 2 provides the “typical” timeframes of recovery following tissue-specific training stress, demonstrating that the recovery of individual tissues to training load (defined as the readiness to receive a similar training stimulus without deleterious local and/or systemic effects) varies markedly. Supercompensation occurs within all tissues, provided that an appropriate amount of recovery is allowed between similar doses of load. It is critical to remember that training provides the stimulus, but adaptation occurs in the recovery window.
How Can Practitioners Know if Their Patients and Athletes Are Adapting (or Maladapting) to Training Stress?
Athlete monitoring can be viewed as a “cycle” – training load is applied, and the response is monitored (Figure 3). If, given an adequate recovery period the response is appropriate, the athlete can perform a similar (or greater) dose of training. However, if the response is poor, then the training load can be adjusted, by either reducing training load, providing more recovery, or making other modifications to the training program. With all the training monitoring technologies now available, it can be overwhelming for practitioners to know what (and how much) to monitor. To minimize the risk of confusion with too much data, practitioners might consider asking “what is the least amount of information I require, in order to make an effective training decision?”
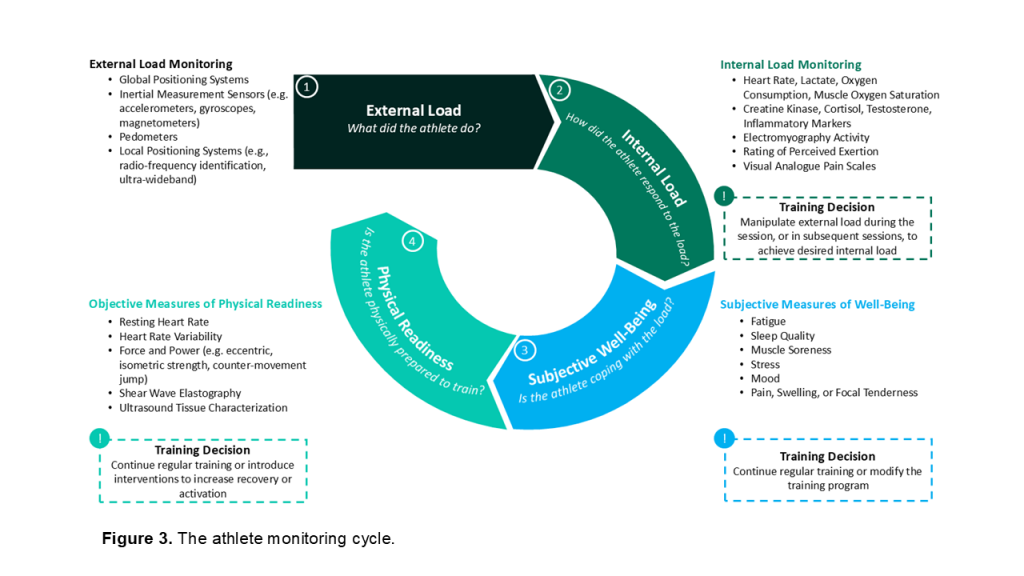
Irrespective of the monitoring tool chosen, it is recommended that practitioners quantify the load applied and the response to that load. For example, if it is important to gain an understanding of an athletes’ recovery following a high-volume sprinting session, and the readiness of that athlete to receive a similar dose of sprinting, practitioners might choose a measure of posterior chain muscle strength, hip and knee joint range of motion, or dynamic lumbo-pelvic control [1]. Note, that the load and response measure will likely differ depending on the tissue and system of interest.
When choosing the monitoring strategy, start with the question: “what do I want to know from monitoring my athlete?”
1. If it’s of interest to understand if the training load is eliciting an appropriate training intensity, monitor the response during the session (e.g. using a pain scale, RPE scale or heart rate monitor);
2. If it’s of interest to know if the athlete is suitably recovered following a training session, monitor the response using a subjective wellbeing scale (e.g. perceptions of fatigue, soreness, stress, etc) or a measure of physical readiness (e.g. counter-movement jump, Wattbike test).
If limited budget and resources are available, the athletes’ load-response can be easily monitored using an RPE and subjective wellbeing scale.
How Do I Make Sense of the Monitoring Data?
An isolated piece of data, without any context is meaningless. High training loads or good wellbeing alone, only provide part of the story. It’s when these data are combined that they can be used by practitioners to inform their training prescription. This ensures data is interpreted within an athlete monitoring framework [2] and assists practitioners decide whether to continue training as planned, adjust training load (i.e. increase or decrease), or investigate other factors that might influence adaptation (e.g. stress, sleep, hydration, nutrition, etc) (Figure 4).
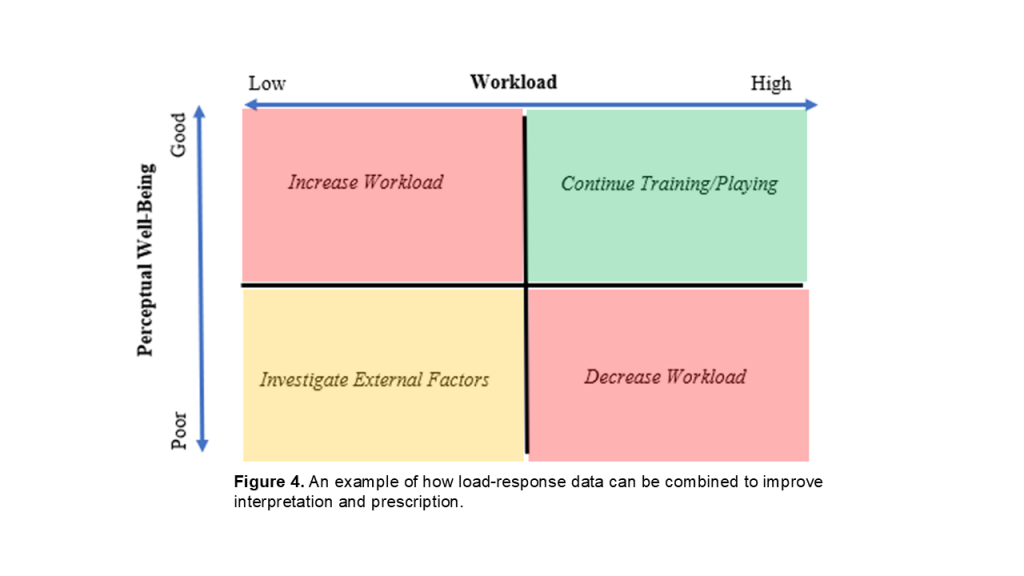
Equally, it is important that data is interpreted within the context of the training program (i.e. “What are we trying to achieve?” “How important is it to return this player to competition quickly?” What stage of the season are we in?”). While it might be ideal to have athletes in a state of readiness when approaching important competitions, it is perfectly reasonable (and expected) for athletes to feel a level of fatigue in pre-season! Finally, it is recommended that practitioners are not overly reactive to changes in the load-response – some daily and weekly fluctuations are normal and expected. Calculating z scores and interpreting the load-response based on an individual athletes’ data is one approach that ensures training prescription is highly individualized.
So, How Can Sports Medicine and Performance Practitioners Use Athlete Monitoring in Their Programs?
Athlete monitoring can take the guesswork out of rehab and peak performance programs. If you are a sports medicine practitioner or strength and conditioning coach, here’s some simple tips to optimize your training programs:
1. Not all tissues respond at the same rate. Considering the tissue load-response within Selye’s general adaptation syndrome framework ensures that appropriate recovery is provided to promote supercompensation at the level of the tissue.
2. An external load monitoring device (e.g. GPS or inertial measurement sensor) does not provide specific information on tissue or system stress. Incorporating a response measure ensures athletes are adapting to the applied training stress.
3. Consider the training adaptation you are trying to elicit, and the tissue(s) you are trying to target. This will help you decide what load and response measures are needed to inform your training prescription.
https://gabbettperformance.thinkific.com/collections
References
- Carmona G, Moreno-Simonet L, Luis Cosio P, Astrella A, Fernandez D, Padulles X, Cadefau JA, Padulles JP, & Mendiguchia J. Acute changes in hamstring injury risk factors following a session of high-volume maximal sprinting speed efforts in soccer players. Sports Health, 2025;17:15-26.
- Gabbett TJ, Nassis GP, Oetter E, Pretorius J, Johnston N, Medina D, Rodas G, Myslinski T, Howells D, Beard A, & Ryan A. The athlete monitoring cycle: A practical guide to interpreting and applying training monitoring data. Br J Sports Med, 2017;51:1451-1452.
- Gabbett TJ & Oetter E. From tissue to system: what constitutes an appropriate response to loading? Sports Med., 2025;55:17-35.
- Selye H, Stress and the general adaptation syndrome. Br Med J. 1950;1383-1392.
- Viru A. Early contributions of Russian stress and exercise physiologists. J. Appl. Physiol., 2002;92:1378-1382.